How computer science and engineering research at Bath is supporting healthcare

Developing markerless motion capture to analyse body movements for sports performance, injury prevention or rehabilitation
Researchers at CAMERA, the University of Bath’s Centre for Analysis of Motion, Entertainment and Research Applications in our Departments of Computer Science and Health, have been developing, validating and applying new technologies to measure motion without the need for markers or any instrumentation to be worn.
Motion analysis traditionally relies on attaching light-reflective markers onto specific points on the body; the movement of these markers in 3D space is then calculated using data from an array of cameras that film the person’s movements from different angles. However, placing markers accurately on the body can be time consuming to set up and can sometimes interfere with the person’s natural movements.
“The trouble with using markers is that they can be tricky to place on a participant accurately and reliably and this process can take a long time, which isn’t very practical for many participants and applications, for example elite athletes or clinical populations.”
To overcome this, the team at CAMERA led by Dr Steffi Colyer have developed non-invasive markerless solutions using computer vision and deep learning methods to measure motion by identifying body landmarks from regular 2D image data.
“These technologies open the door for us to capture motion data more readily in settings outside of the laboratory and importantly the outcomes for the movements we have analysed are comparable to traditionally used techniques with markers,” she says.
“This could be useful for physiotherapists, clinicians and sports trainers in a wide range of applications including sports performance and injury prevention or rehabilitation.”
Dr Steffi Colyer, Senior Lecturer in the Department for Health.
Dr Steffi Colyer, Senior Lecturer in the Department for Health.
At the University of Bath, the system has been used to measure the biomechanics of skeleton athletes during their push-starts, providing new insights to the Great British team in their preparations for the 2026 Winter Olympic Games in Milano Cortina. Additionally, Dr Colyer and colleagues have used the technology to unobtrusively monitor how much work racket sport (tennis and badminton) players are performing during training and match play, and to measure the biomechanics of Olympic weightlifting.
Researchers at the University of Bath have been working with GB skeleton athletes based at the Team Bath Sports Training Village.
Researchers at the University of Bath have been working with GB skeleton athletes based at the Team Bath Sports Training Village.
This technology has huge potential in healthcare settings as well. By analysing movement in near real time, markerless motion capture can streamline data collection and offer immediate feedback on how someone’s movement changes, both across multiple sessions, and within a single session. Dr Logan Wade and colleagues have been developing a low-cost system that uses high-speed web-cameras, aiming to put this powerful tool in the hands of coaches, clinicians and researchers around the world.
Dr Logan Wade, Research Fellow in the Department for Health.
Dr Logan Wade, Research Fellow in the Department for Health.
“I’m incredibly excited to finally take motion capture out of the lab and put it in the hands of everyday users,” says Dr Wade. “This technology will allow biomechanical data to be collected at a scale we’ve never seen before, transforming how we monitor, understand, and ultimately prevent injuries and support rehabilitation in all areas of life.”
Learn more about Bath research in our monthly email

Dame Professor Angela Mclean, Government Chief Scientific Advisor, speaking with Dr George Stothart about his research when she visited the University of Bath this year.
Dame Professor Angela Mclean, Government Chief Scientific Advisor, speaking with Dr George Stothart about his research when she visited the University of Bath this year.
Detecting Alzheimer’s years before clinical diagnosis
Dementia is currently diagnosed too late, up to 20 years after the disease has begun. With the development of the breakthrough drugs donanemab and lecanemab, likely to be most effective in the early stages of Alzheimer’s, an early diagnosis is more important than ever before. Quicker, more accurate ways to diagnose dementia are greatly needed so patients can get treatments earlier and plan for their future.
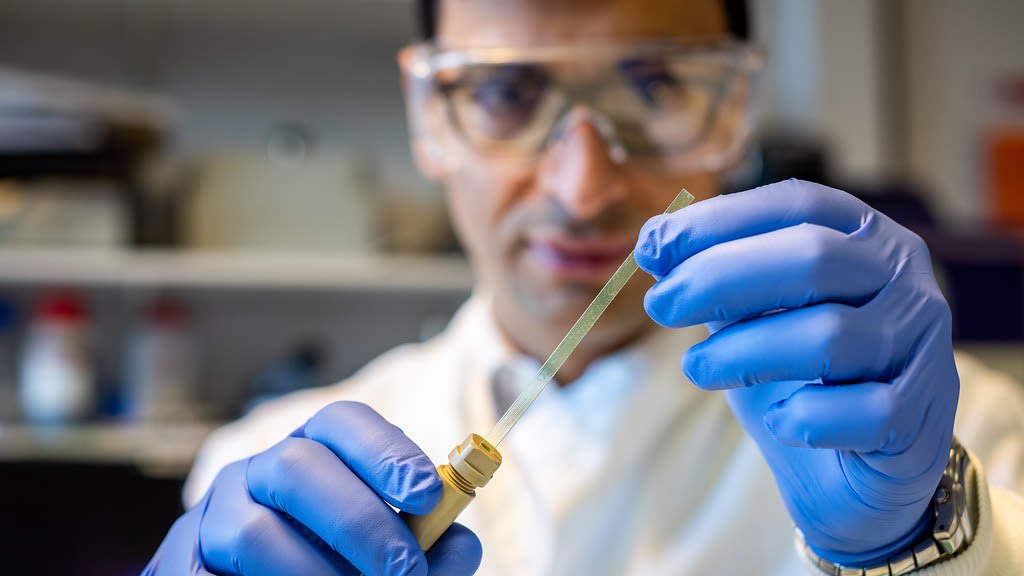
George Stothart, a cognitive neuroscientist in the Department of Psychology at the University of Bath, alongside researchers from the University of Bristol, has successfully trialled ‘Fastball’, a simple brainwave test for memory decline which has been shown to detect signs of memory impairment linked to Alzheimer’s disease years before clinical diagnosis is typically possible.
Published in the journal Brain Communications, his study reports that this three-minute passive test - which records electrical activity in the brain while participants view a stream of images - can reliably identify memory problems in people with Mild Cognitive Impairment (MCI); a condition that can lead to Alzheimer’s. This follows his previous study in 2021 that demonstrated Fastball was sensitive to memory impairment in Alzheimer’s disease.
Dr Stothart says Fastball could be scaled for use in GP surgeries and memory clinics. Crucially, the research has demonstrated that the test can be administered in people’s homes, outside of a clinical environment, opening the door to wider screening and monitoring using accessible, low-cost technology.
“We’re missing the first 10 to 20 years of Alzheimer’s with current diagnostic tools.
Fastball offers a way to change that – detecting memory decline earlier and more objectively, using a quick and passive test. There’s an urgent need for accurate, practical tools to diagnose Alzheimer’s at scale. Fastball is cheap, portable, and works in real-world settings.”


The study was funded by the Academy of Medical Sciences and supported by dementia research charity BRACE. Chris Wiliams, CEO of BRACE Dementia Research, said:
“Fastball is an incredible tool that could offer anyone who, for whatever reason, cannot access a dementia diagnosis in a clinical setting. BRACE has been supporting the development of Fastball for several years, and we are excited to see what Dr Stothart’s team will achieve over the next few years with ongoing support from the charity.”
Dr Stothart's research has enabled him to partner with industry through an NIHR Invention for Innovation (i4i) grant. Working with global digital health company Cumulus Neuroscience, he is part of the Global Alzheimer’s Platform Foundation (GAP) Bio-Hermes 2 Study. This is generating data to accelerate the adoption and effective use of biomarkers in the study of Alzheimer’s disease. Dr Stothart, who is also a Principal Scientist at Cumulus, says: “Dementia diagnosis is a global challenge and one best met with cooperation and combined efforts of clinical research and industry."
Computer science research at the University of Bath
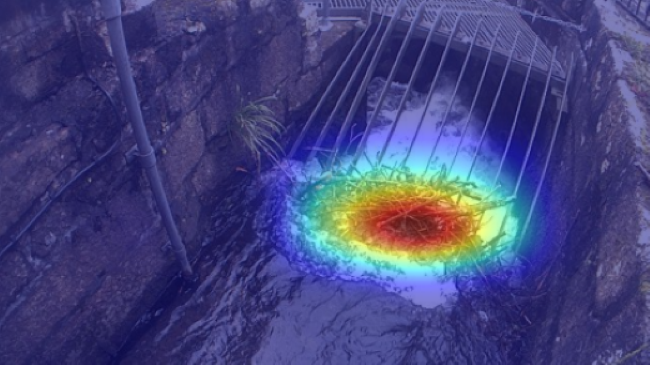
The ‘AI on The River’ software is trained to accurately detect debris blocking culvert trash screens
The ‘AI on The River’ software is trained to accurately detect debris blocking culvert trash screens
Extreme weather events driven by climate change are intensifying, and have the potential to wreak havoc around the world, particularly in economically disadvantaged areas
Extreme weather events driven by climate change are intensifying, and have the potential to wreak havoc around the world, particularly in economically disadvantaged areas
Race Yourselves! launched on Meta Quest Store with AI and VR innovations
Race Yourselves! launched on Meta Quest Store with AI and VR innovations
How the Centre for Bioengineering and Biomedical Technologies is supporting healthcare
The Centre for Bioengineering and Biomedical Technologies (CBio) at the University of Bath addresses challenges in human health and wellbeing through transdisciplinary and translatable bioengineering research.
“The COVID-19 pandemic brought into sharp focus the fragility of health systems even in developed countries,” states Centre Director, Professor Pedro Estrela. “This has accelerated efforts towards decentralised health monitoring, personalised treatments, and the integration of electronic and digital systems in both care delivery and disease management. CBio is at the forefront of addressing these challenges.”
Work at CBio spans a range of projects, from biosensors and lab-on-chip devices for medical applications, to environmental monitoring of wastewater and soil, and biomechanical orthopaedics and bioprocess engineering. “We are a diverse, collaborative and inclusive community delivering impact through innovation in the areas of targeted and personalised interventions, sustainable healthcare, and humans and the environment,” explains Professor Estrela.
“We aim to merge areas that don't normally intersect and tackle head-on the global challenges in human health, environmental sustainability, and industrial bioprocesses.”

The Ultrasound Computed Tomography belt could make monitoring patients with heart and lung conditions easier.
The Ultrasound Computed Tomography belt could make monitoring patients with heart and lung conditions easier.
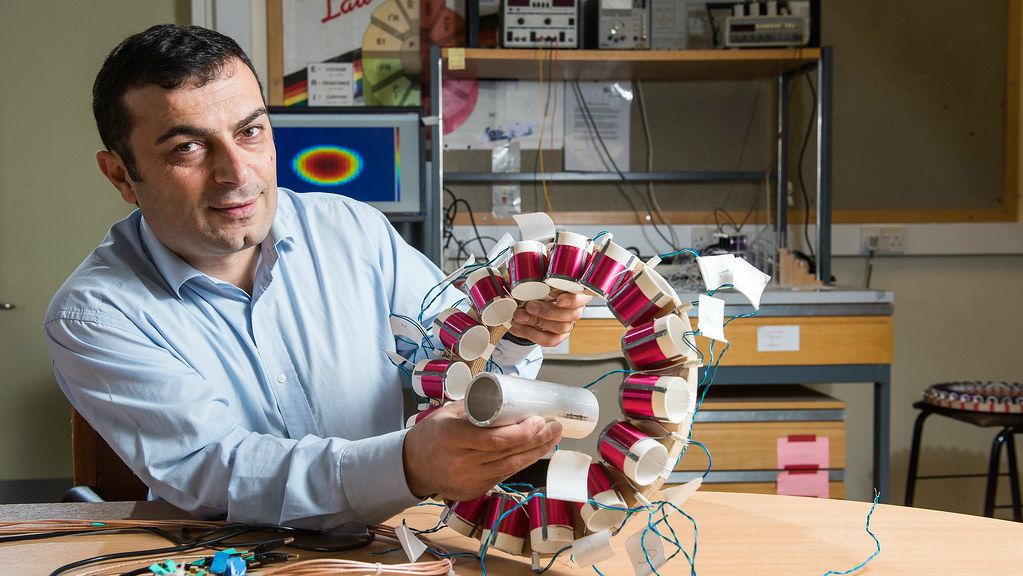
Professor Manuch Solemani is a core member of CBio and leads the University of Bath's Engineering Tomography Laboratory.
Professor Manuch Solemani is a core member of CBio and leads the University of Bath's Engineering Tomography Laboratory.
New wearable device that mimics CT scans for heart and lung patient monitoring
Currently, patients with conditions such as heart failure, pneumonia, or respiratory distress often require multiple imaging procedures that are intermittent, disruptive, and radiation intensive. Researchers in CBio have developed a first-of-its-kind wearable device for patients capable of continuously scanning the lungs and heart of hospital patients while they rest in bed.
The belt-like device, attached around a patient’s chest, uses ultrasound and works like a CT scanner. Rather than taking an isolated snapshot, it can produce a series of dynamic, high-resolution images of the heart, lungs and internal organs over time, giving doctors deeper insight into a patient’s condition.
Professor Manuch Soleimani, lead author of the research paper, is based in Bath’s Department of Electronic & Electrical Engineering and leads the University’s Engineering Tomography Lab. He says:
“This could fundamentally change how we monitor patients in critical care or post-surgical settings. The imaging quality of the device can be on par with an X-ray or CT scan, but instead of a single snapshot, we can monitor how the lungs and heart behave over time, which is far more informative when managing dynamic conditions.”
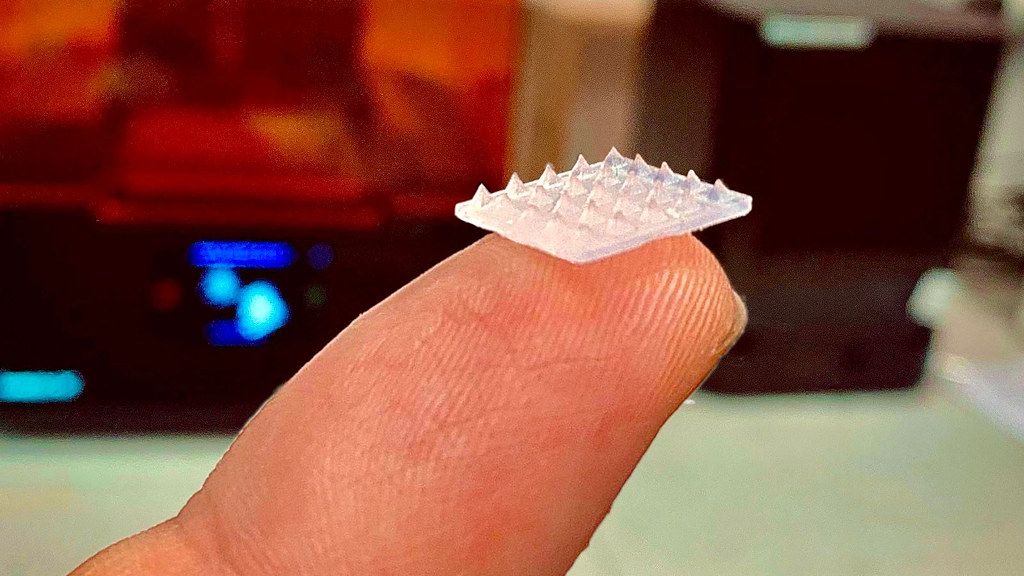
Removing the need for needles with a new skin patch alternative for drug delivery
An affordable microneedle skin patch that delivers a controlled dosage of medicine directly into the body, eliminating the need for injections or oral medication, has been developed by a team led by scientists at CBio.
“Injections are invasive and expensive, and they don’t suit everyone,” says Dr Hannah Leese, a Chemical Engineer at the University of Bath. “A lot of people are needle-phobic and are understandably reluctant to receive medicine by injection even when treatment is really needed. Others are ill-suited to injections – for instance, elderly patients with thin skin.”
The microneedle patch developed at Bath is made from a hydrogel (a gel-like substance in which water forms the liquid component), with the active ingredient encapsulated inside the hydrogel microneedle structure rather than in a separate reservoir. They are also more affordable than other commercially available microneedle patches, as they are produced from 3D printed moulds. Moulds produced this way are easy to customise, which keeps costs down.

Collaborating with RUH clinicians for new medical device to improve accuracy of drilling screw holes into bones during surgery
A ground-breaking new medical device developed by Dr Ioannis Georgilas, a senior lecturer in Mechanical Engineering and CBio member, improves the accuracy of drilling screw holes into bones during surgery.
The drill guidance system (DGS), which has been developed alongside RUH staff, helps surgeons to be even more accurate when drilling holes, reducing the time patients spend in the operating theatre. When fixing a break in the bone that requires a screw fixing, the surgeon will normally use just their eyesight and x-rays when directing the drill to make the hole.
Using the drill guidance system, the surgeon uses all the same techniques but with the addition of a camera on the drill and an indicator which helps them guide the drill in the correct direction as it passes through the bone. The increased accuracy the DGS provides helps to reduce the number of x-rays a patient needs as well as enabling a single-attempt approach to drilling, reducing bone and soft-tissue damage, and chances of infection.
Since it was introduced, the DGS has been used in operations on wrists, arms, knees and ankles because of both trauma and planned surgery. It is hoped that the device will be used in even more operations in the future.
The project at the RUH is being led by Professor Grey Giddins, a Consultant Orthopaedic and Hand surgeon, with support from Dr Georgilas.
Professor Giddins said: “The use of the drill guidance system for the first time during surgery is fantastic news and really will improve the experiences of the people we care for, reducing the amount of time they spend in surgery as well as reducing the chances of infection.
“The development and successful clinical implementation of the Drill Guidance System represents a significant advancement in medical device development, enhancing surgical precision and patient care.”
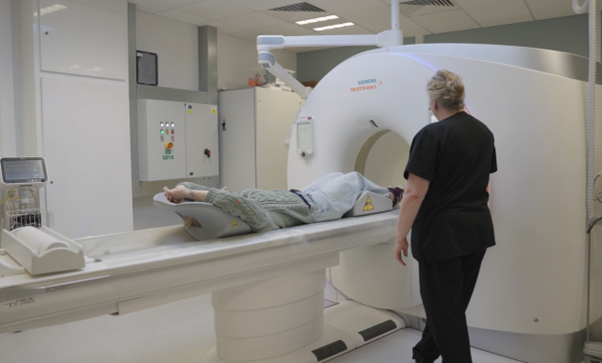
University of Bath and RUH working together to improve diagnosis and treatment of pulmonary embolic disease
Pulmonary embolic disease occurs when blood clots block arteries in the lungs. Some patients go on to develop the long-term condition Chronic Thrombo-Embolic Pulmonary Hypertension (CTEPH). Both conditions can be life-threatening if not identified and treated promptly.
An ongoing collaboration between the University of Bath’s Department of Mechanical Engineering and the Royal United Hospital (RUH), is investigating how AI can be used to improve diagnosis and treatment for patients with pulmonary embolic disease.
Through this joint research, Bath engineers and RUH clinicians are developing and testing AI software that could help spot these conditions earlier, enabling patients to receive the right treatment sooner and improving outcomes.
The project is led by Dr Jonathan Rodrigues, Consultant Cardiothoracic Radiologist at the RUH, and the engineering aspects are managed by Dr Andrew Cookson, Department of Mechanical Engineering at the University of Bath and CBio member. Dr Lisa Austin is supporting the patient and public involvement aspects with colleagues from the Department for Health.
“We hope that by working with our AI partners, using the very latest artificial intelligence tools, we can help to save lives and get the very best value for money for the NHS.”
Our research is helping to improve the world. Through collaborative partnerships we're creating a healthier, more sustainable, and connected future for all.