Science Meets Policy
How Bath research in chemistry and biology is helping to prepare for global health emergencies

“It is not a question of ‘if’ another pandemic will strike, but when", wrote Baroness Hallett in the first report of the UK Covid-19 enquiry. “Preparedness for and resilience to a whole-system civil emergency must be treated in much the same way as we treat a threat from a hostile state.”


At the University of Bath, our researchers are working to help inform policy in preparation for future health emergencies. Across the University, teams are collaborating with a range of partners and stakeholders, including industry, the UK government, hospitals, the police, and other leading universities to help prepare the world for the next global health crisis.
“Our work is all part of a wider push to be ready for the next pandemic,” said Dr Asel Sartbaeva. “The government wants to be in a position to act fast with vaccine rollouts next time.”
Dr Asel Sartbaeva is the CEO and Co-Founder of EnsiliTech, a University of Bath biotech spinout that has developed technology which allows vaccines and other biological materials to be transported and stored without the use of refrigeration.
Despite modern advances in how vaccines are manufactured, the transportation of biopharmaceuticals relies on a 50-year-old global ‘cold chain’ system; a costly and energy-intensive system for refrigeration and freezing during transit and storage, Cold chain failures resulting in spoiled stock are reported to cost the pharmaceutical industry an estimated £26 billion annually. In developing economies, the World Health Organization (WHO) reports that up to 50% of vaccines are wasted due to cold chain breakdowns, leaving millions without access to vital treatments.
The mission of EnsiliTech, says Asel, is to ensure that life-saving medicines and vaccines reach everyone, everywhere, regardless of infrastructure or geography.
EnsiliTech’s patented technology preserves the integrity of vaccines, antibodies, and other biopharmaceuticals, eliminating the need for a cold chain and allowing medicines to be stored and transported at temperatures of up to 50°C. This means that life-saving medicines can be transported anywhere across the globe, particularly to underserved regions where access to reliable refrigeration can be a major barrier to healthcare.

"By eliminating the need for refrigeration, our technology significantly reduces supply-chain costs and drug waste, while also lowering the environmental impact of pharmaceutical distribution.” -
The potential for this work to help ameliorate and prevent global health emergencies is clear and in 2024, EnsiliTech was awarded a highly competitive UK government contract of £1.7 million to develop the world's first thermally stable mRNA vaccine. mRNA vaccines have a huge potential to prevent not only infectious diseases but also certain cancers and a range of other previously unpreventable conditions. However, these vaccines currently require ultracold storage, needing to be kept at -80 °C.
"Our vision is for a more equitable and sustainable future in global healthcare," says Asel. Earlier this year, the company raised its second oversubscribed funding round, securing £4.5 million in seed funding, which promises to make her aim a reality.
Dr Asel Sartbaeva
Dr Asel Sartbaeva
Dr Asel Sartbaeva
Dr Asel Sartbaeva
Learn more about Bath research in our monthly email

Spotting the next
epidemic in wastewater
While Asel’s work is ensuring vaccines reach people in time, research in another part of the University is focused on the adage that prevention is better than cure.
Professor Barbara Kasprzyk-Hordern, who leads the new Centre of Excellence in Water-Based Early-Warning Systems for Health Protection (CWBE) at the University, is working to help authorities sooner identify and react to public health emergencies.
“The trouble with monitoring public health using traditional epidemiology studies is that they rely on people filling out surveys or providing samples,” she says. “Unfortunately, surveys have limitations in terms of accuracy of the data provided by individuals as well as the timescales required to collect such data.”
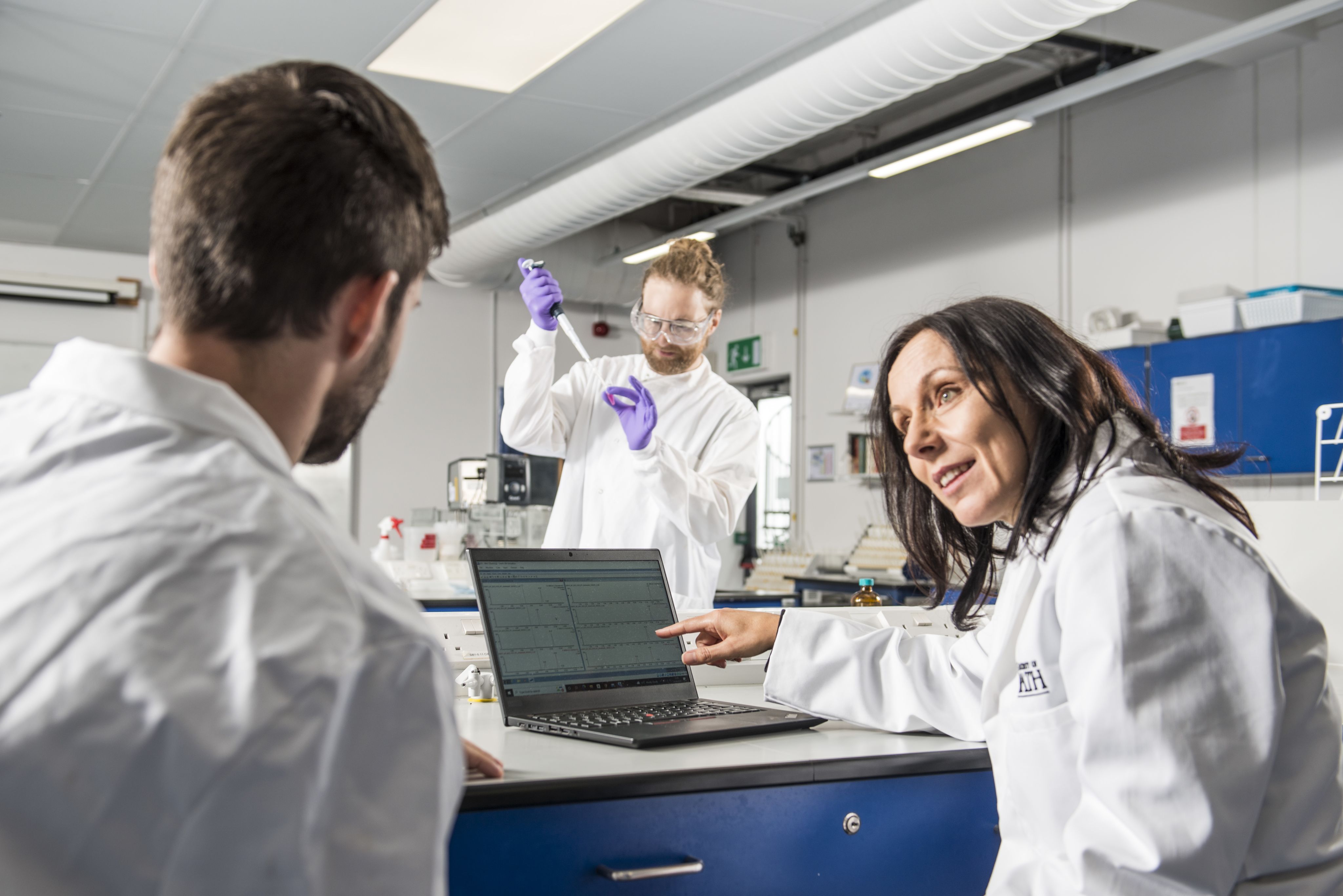
Working with the water industry and the UK Health Security Agency, Barbara and her team are piloting the first large-scale UK public health surveillance system to analyse wastewater. Routine monitoring at sewage treatment works could provide a powerful early warning system for the next flu or norovirus epidemic, alerting hospitals to prepare and providing public health agencies with vital health information.
She says: “Our study has shown that only 10 daily samples from 10 wastewater treatment plants are needed to provide anonymous and unbiased information on the health of 7 million people - this is much cheaper and faster than any clinical screening process. This could, therefore, potentially be a very powerful tool for giving a holistic understanding of public health of different communities.”
Investigating fungal 'superbugs' in hospitals and the environment
Work to help prevent the rapid spread of disease is also taking place in the University’s Milner Centre for Evolution.
The risk of pathogenic fungi in hospitals and the environment is a growing global public health concern. Pathogenic fungi cause 13 million infections and around 1 million deaths around the world every year. The genus Candida contains numerous pathogenic species, including C. albicans, C. auris and C. parapsilosis, which can cause hospital outbreaks. In much the same way that bacteria are becoming increasingly resistant to antibiotics, these fungi are commonly resistant to antifungal drugs. This makes infections difficult to treat and control.
Professor Edward Feil from the Milner Centre and the Department of Life Sciences has been awarded €2.3 million (£1.9 million) to lead a research group from across Europe and Australia to understand and manage the spread of these pathogenic fungi in hospitals and the environment.
His team will use genome sequencing to identify fungal strains that have become adapted to the hospital environment, in a way that is similar to the familiar bacterial ‘superbugs’ like MRSA, while also working with the Centre of Excellence in Water-Based Early Warning Systems for Health Protection to analyse wastewater samples. This will allow them to determine how frequently these strains might be carried by healthy individuals in the community.
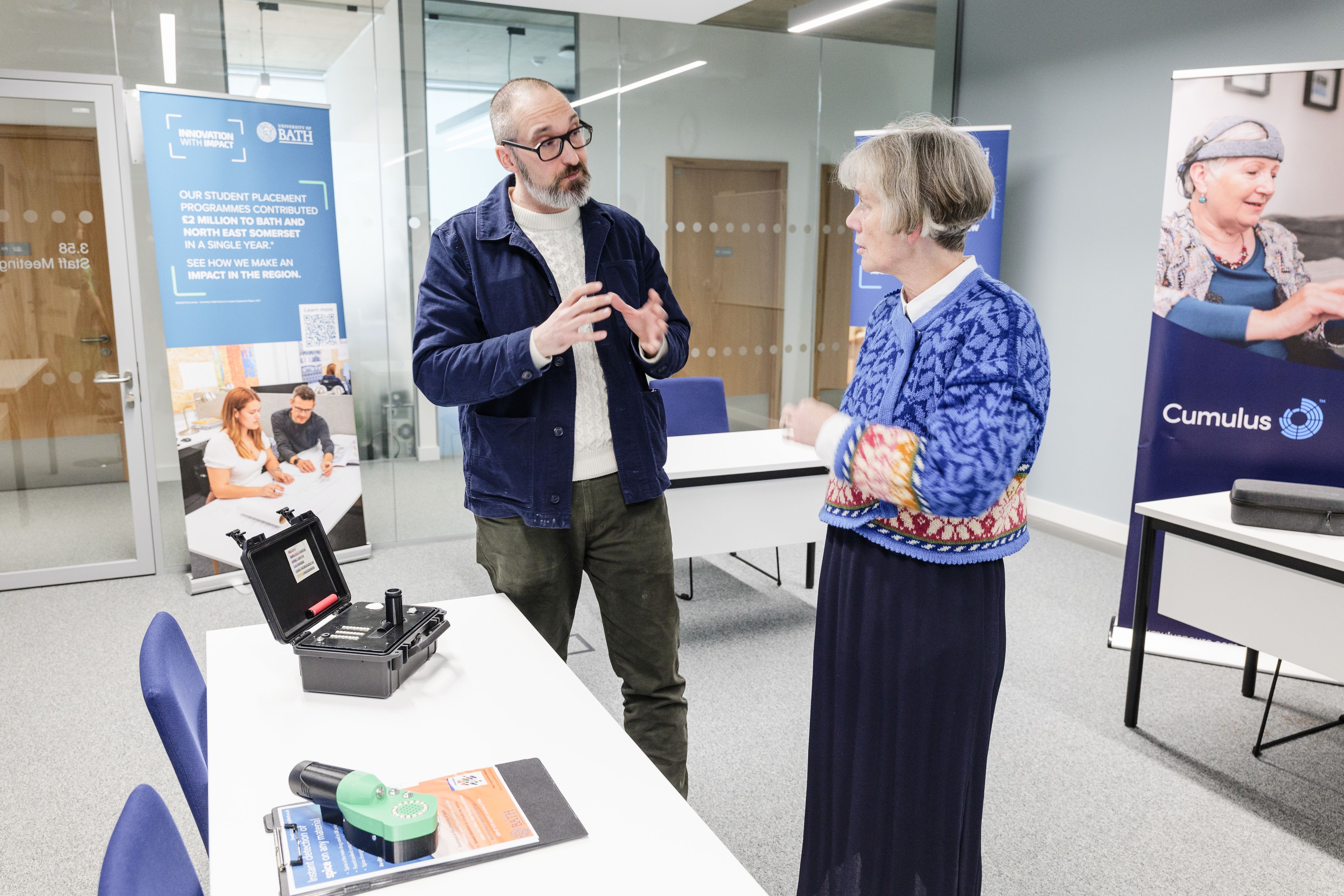
A visit to University of Bath’s Centre for Excellence in Water-Based Early Warning Systems by Chief Scientific Adviser Professor Dame Angela McLean (2nd left) to see work, led by Prof Ed Feil (2nd right) and Prof Julie Barnett (3rd right)
A visit to University of Bath’s Centre for Excellence in Water-Based Early Warning Systems by Chief Scientific Adviser Professor Dame Angela McLean (2nd left) to see work, led by Prof Ed Feil (2nd right) and Prof Julie Barnett (3rd right)
“It’s an outstanding opportunity to work with some of the best genomics experts across Europe, and to generate data that will further our understanding of how these dangerous pathogenic fungi are spreading through hospitals, so informing more effective disease management strategies.”

Professor Chris Budd OBE receives award for Covid-19modelling work
Professor Chris Budd OBE, Department of Mathematical Sciences, is another pioneering academic at the University whose research ensured government had access to world-leading scientific evidence during the pandemic.
At various points, Professor Budd’s models helped inform government policy on safe ways for people to congregate when attending university lectures, travelling by public transport or gathering for large events.
In 2022, he received an Award for Modelling & Data Support from the British government for his ‘exceptional contribution’ to epidemiological and modelling work. Accepting the award, he said: “It’s an honour to receive this accolade, and an equal honour to have been part of a fantastic team here at Bath doing our part to fight Covid.”
Research at Bath is addressing looming public health emergencies
Health and biology research at Bath is not just preparing for the next pandemic and academics in the Centre for 21st Century Public Health are looking to drive meaningful change at local, national, and international levels to improve human health. Members of the team have spoken at the World Health Organisation, the United Nations and Climate Week NYC about their work to address the prevention and control of noncommunicable diseases (NCDs) and the promotion of mental health and wellbeing, many of which were exacerbated by the Covid-19 pandemic.
As Director of the Centre for Motivation and Behaviour Change, Professor Martyn Standage has been exploring how pandemic-influenced lifestyles, including increased screen time and a decline in physical activity, are contributing to a childhood inactivity crisis. He was one of the lead authors in a 2022 report by the Active Healthy Kids Global Alliance (AHKGA) involving 682 experts from 57 countries that assessed global levels and trends in child and adolescent physical activity.
“New habits have been formed by children and adolescents around the world in response to the new normal provoked by a socially accepted screen-centric indoor living society and exacerbated by the COVID-19 pandemic, global conflicts, and severe weather associated with climate change.”
Martyn’s work highlighted that modern lifestyles – including increased digital screen time, the growing urbanisation of communities, and the rise in automation of previously manual tasks – contribute to a pervasive yet unequally distributed public health problem that must be recognised as a global priority.
“Policymakers worldwide continue to struggle with rising inactivity among youth. Our data calls for coordinated, evidence-based interventions that can effectively counter the sedentary pull of modern life.”

Detecting synthetic drugs in vapes
Meanwhile, Professor Chris Pudney is leading the charge on an emerging public health crisis affecting children throughout the country. After work in developing the world’s first device to detect Spice, a synthetic prison drug that can cause a wide range of dangerous side effects, including cardiac arrest, Chris was approached by schools across the UK to test confiscated vapes suspected of containing the same substance.
After analysing 1,923 e-cigarettes and e-liquids collected from 114 schools across seven regions in England, he found that one in four vapes confiscated in secondary schools contained Spice.
“We know children can have cardiac arrests when they smoke spice, and I believe some have come quite close to death. Headteachers are telling me pupils are collapsing in the halls and ending up with long stays in intensive care.” – Professor Chris Pudney
Chris's work has revealed that Spice-laced vape liquids are easily available online in a widespread and overt market on social media platforms, where the products are often deceptively marketed as ‘THC’ vapes, despite containing Spice. "Teenagers think they are purchasing vapes or vape fluid containing THC or nicotine when, in fact, they are laced with spice,” he says. “Education of young people, teachers and parents on this issue is the first key step in mitigating the risk from this emerging threat.”
Over 2025, Professor Pudney has engaged with social media companies to make them aware of this issue, collaborating with the drug education charity, Daniel Spargo-Mabbs Foundation, and the research has been raised in parliaments in the UK and abroad.
Speaking about the impact he hopes to see because of the research, Chris says, “This is a failure of online safety that is causing direct harm to children. The Online Safety Act needs to be used to compel social media companies to find and remove the accounts selling these drugs to children. We are calling for Ofcom to be properly resourced and directed to open a specific enforcement programme dedicated to online drug sales.”
Chief Scientific Adviser Professor Dame Angela McLean meets Professor Chris Pudney
Chief Scientific Adviser Professor Dame Angela McLean meets Professor Chris Pudney
Professor Chris Pudney
Professor Chris Pudney
Bath MP Wera Hobhouse raises Bath research in Parliament which found that the synthetic street drug Spice was being sold in vapes and being used by children.
Our research is helping to improve the world. Through collaborative partnerships we're creating a healthier, more sustainable, and connected future for all.